

Comparisons of categorical data were conducted with a Fisher’s exact test. Continuous and categorical data were summarized with descriptive statistics. To ensure adequate assessment of MRD, over-enrollment was allowed. 26 For mITT, patients who failed to achieve a very good partial response (VGPR) or better or who did not complete KRd treatment for any reason were considered MRD positive, and patients who achieved a VGPR or better but did not have evaluable MRD were excluded from the analysis. The MRD rate was estimated for the evaluable population and for a modified ITT (mITT) population as described by Perrot et al. For all other efficacy analyses, including time-to-event end points and safety, the results are based on the intent-to-treat (ITT) population, defined as all patients who received at least 1 dose of carfilzomib and lenalidomide. Patients who received <4 cycles of KRd consolidation were evaluable for the primary end point. 7,8,17,22įor the primary efficacy analysis, all patients were evaluated except those who declined to receive ASCT for reasons other than toxicity or efficacy. 19-21 In studies of patients undergoing transplantation with multidrug induction and consolidation, the duration of triplet regimens such as RVd and KRd has generally been limited to 3 to 6 cycles of induction with 2 to 4 cycles of consolidation. Although the optimal duration of initial treatment is not well established, recent studies in transplant-ineligible patients indicate that extended treatment improves disease control compared with shorter, fixed durations, although a significant overall survival (OS) benefit has not been demonstrated. 17 In addition, there is emerging evidence that duration of treatment with multidrug regimens plays a role. 14-18 Results from randomized trials have shown that incorporation of ASCT into RVd treatment improved clinical outcomes compared with RVd without ASCT, which supports the use of ASCT with novel regimens as a standard of care. Ongoing efforts to further improve treatment outcome in patients with NDMM include incorporation of monoclonal antibodies 12-14 and/or autologous stem cell transplantation (ASCT) into treatment with novel regimens.
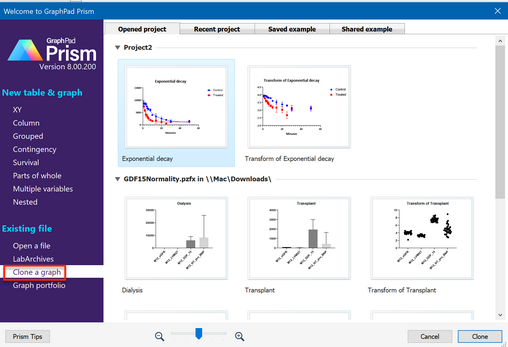
#CANCEL GRAPHPAD FREE TRIAL TRIAL#
This trial was registered at as #NCT01816971.
Extended KRd maintenance after consolidation contributed to deepening of responses and likely to prolonged PFS and OS. Patients with NDMM treated with KRd with ASCT achieved high rates of sCR and MRD-negative disease at the end of KRd consolidation.

There was no grade 3 to 4 peripheral neuropathy. Grade 3 to 4 adverse events included neutropenia (34%), lymphopenia (32%), infection (22%), and cardiac events (3%). For high-risk patients who were MRD negative, 5-year rates were 77% and 81%. After median follow-up of 56 months, 5-year progression-free survival (PFS) and overall survival (OS) rates were 72% and 84% for ITT, 85% and 91% for MRD-negative patients, and 57% and 72% for patients with high-risk cytogenetics. The rate of minimal residual disease (MRD) negativity using modified ITT was 70% according to next-generation sequencing (<10 −5 sensitivity). On intent-to-treat (ITT), the sCR rate reached 76%. The primary end point was met, with an sCR rate of 60% after 8 cycles. Seventy-six patients were enrolled with a median age of 59 years (range, 40-76 years), and 35.5% had high-risk cytogenetics. The primary end point was rate of stringent complete response (sCR) after 8 cycles of KRd with a predefined threshold of ≥50% to support further study. Transplant-eligible patients with NDMM received 4 cycles of KRd induction, ASCT, 4 cycles of KRd consolidation, and 10 cycles of KRd maintenance. In this phase 2 multicenter study, we evaluated the incorporation of autologous stem cell transplantation (ASCT) into a carfilzomib-lenalidomide-dexamethasone (KRd) regimen for patients with newly diagnosed multiple myeloma (NDMM).


 0 kommentar(er)
0 kommentar(er)
